Part 1
 By Dr Vineet Naja, MS (General Surgery) MCh (Urology)
By Dr Vineet Naja, MS (General Surgery) MCh (Urology)
(Consulting Urologist and Andrologist)
Prostate problems are common male health problem. For men under 50, the most common prostate problem is prostatitis. For men over 50, the most common prostate problem is prostate enlargement, also called benign prostatic hyperplasia (BPH). Older men are at risk for prostate cancer as well, but this disease is much less common than BPH. This article will be in two parts. This part covers some general information about prostate, prostatitis and carcinoma prostate. Next week’s article will cover the more common prostate enlargement (BPH) problem.
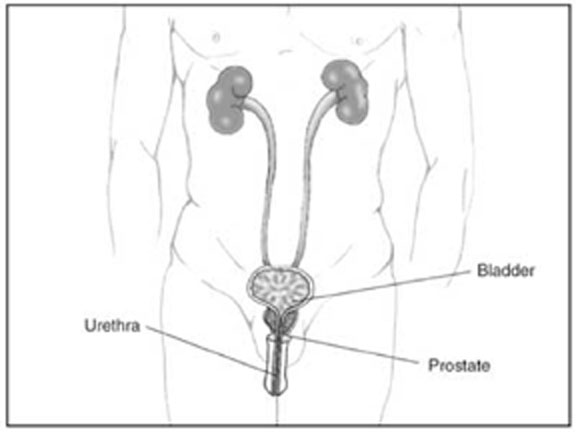
The prostate gland
The prostate is a walnut-shaped gland located below the bladder (where urine is stored) and in front of the rectum. It wraps around the urethra (the tube that carries urine through the penis). The entire prostate gland is surrounded by a dense, fibrous capsule. Scientists do not know all the prostate’s functions. One of its main roles, though, is to produce a milky fluid, and during sex the smooth muscles contract and squeeze this fluid into the urethra. Here, it mixes with sperm and other fluids to make semen.
The prostate gland undergoes many changes during the course of a man’s life. At birth, the prostate is about the size of a pea. It grows only slightly until puberty, when it begins to enlarge rapidly, attaining normal adult size and shape, about that of a walnut, when a man reaches his early 20s. The gland generally remains stable until men reach their mid-40s, when, in most men, the prostate begins to enlarge again through a process of cell multiplication.
What is prostatitis?
Prostatitis means the prostate might be inflamed or irritated. If you have prostatitis, you may have a burning feeling when you urinate, or you may have to urinate more often. You may also have a fever or you may feel tired.
 Inflammation in any part of the body is usually a sign that the body is fighting germs or repairing an injury. Some kinds of prostatitis are caused by bacteria, tiny organisms that can cause infection or disease. If you have bacterial prostatitis, your doctor can look through a microscope and find bacteria in a sample of your urine. Your doctor can then give you an antibiotic, a medicine that kills bacteria.
Inflammation in any part of the body is usually a sign that the body is fighting germs or repairing an injury. Some kinds of prostatitis are caused by bacteria, tiny organisms that can cause infection or disease. If you have bacterial prostatitis, your doctor can look through a microscope and find bacteria in a sample of your urine. Your doctor can then give you an antibiotic, a medicine that kills bacteria.
Most of the time, doctors don’t find any bacteria in men with prostatitis. If you have urinary problems, the doctor will look for other possible causes, such as urethral stricture, kidney stone or cancer. If no other causes are found, the doctor may decide that you have a condition called nonbacterial prostatitis. Changing your diet or taking warm baths may help. Your doctor may give you a medicine called an alpha-blocker to relax the muscle tissue in the prostate. No single solution works for everyone with this condition. You may have to work with your doctor to find a treatment that’s right for you.
What is carcinoma prostate?
Prostate cancer is a malignant tumour that arises in the prostate gland. As with any cancer, if it is advanced or left untreated in early stages, it may eventually spread through the blood and lymph fluid to other organs. Fortunately, prostate cancer tends to be slow growing compared to other cancers. More than 90% of all prostate cancers remain dormant and clinically unimportant for decades. Most older men eventually develop at least microscopic evidence of prostate cancer, but it often grows so slowly that, many men with prostate cancer “die with it, rather than from it.” The major risk factors for prostate cancer are age, family history, and ethnicity. Male hormones (androgens), particularly testosterone, play a role in the development or aggressiveness of prostate cancer.
What are the symptoms of carcinoma prostate?
Prostate cancer usually causes no symptoms in the early stages. As the malignancy spreads, it may constrict the urethra and cause urinary problems. Significant pain in one or more bones may indicate the occurrence of metastases (spread of disease). This chronic pain occurs most often in the spine and sometimes flares in the pelvis, the lower back, the hips, or the bones of the upper legs. It may be accompanied by significant unexplained weight loss and fatigue.
Diagnosis of carcinoma prostate
Measuring PSA (Prostate specific antigen, a blood test to detect carcinoma prostate) levels increases the chance for detecting the presence of cancer when it is microscopic. The test is not accurate enough to either rule out or confirm the presence of cancer. PSA levels can be increased by various factors other than prostate cancer, including benign prostatic hyperplasia, prostatitis, advanced age, and ejaculation within 48 hours of the test. If cancer is suspected, the doctor will order a biopsy. Only a biopsy, in which a tiny sample of prostate tissue is surgically removed, can actually confirm a diagnosis of prostate cancer. A biopsy is usually performed to confirm or rule out cancer based on a combination of PSA test levels, findings on the DRE (digital rectal examination), family history, and patient’s age and ethnicity.
Staging and treatment options
Because so many prostate tumours are low-grade and slow growing, survival rates are excellent when prostate cancer is detected in its early stages. If the disease is at the locally-advanced stage, in which it has spread beyond the prostate but only to nearby regions, it is more difficult to cure, but survival rates can be prolonged for years in many men. If prostate cancer has spread to distant organs (metastasized), average survival time is 1-3 years, but some of these patients may live much longer.
Treatment choices are generally based on the patient’s age, the stage and grade of the cancer, overall health status, and the patient’s personal preferences for the risks and benefits of each therapy. The options available are:
Surgery (radical prostatectomy) – Removal of the prostate gland. The vessels that carry semen and surrounding tissue may also be removed. Studies indicate that compared to watchful waiting; radical prostatectomy may lower the risk of cancer recurrence and death, particularly for younger men with aggressive tumours. It is usually not appropriate for older men. Radical prostatectomy may be done either through open surgery or laparoscopic techniques.
Radiation therapy targets the tumour either externally (external beam radiation) or internally (implanted “seeds”).
Androgen deprivation therapy also called hormone therapy uses orchiectomy (surgical removal of the testicles) or drugs to stop production of male hormones.
Prostate cancer that does not respond to hormonal treatment is called hormone-resistant, or hormone-refractory, cancer. Chemotherapy may be used to treat hormone-resistant cancer.