There are some unsung heroes who we see every day but often do not recognize them for who they are. We see them in buses, we see them waiting on the streets (sometimes in inclement weather) hoping to get to work and of course we see them in hospitals, health centres and clinics.
These are the heroes who comfort us when we are sick and hospitalized. They are the ones who become our friends when we are at our most vulnerable. Some may have had experiences that were not as romantic as just described or even horror stories to tell, but the majority of these heroes do yeoman service every day.
Nurses are heroes. Often, they are overshadowed by doctors who are seen as the miracle workers but with the advent of the COVID-19 pandemic many are seeing how vital these frontline workers are.
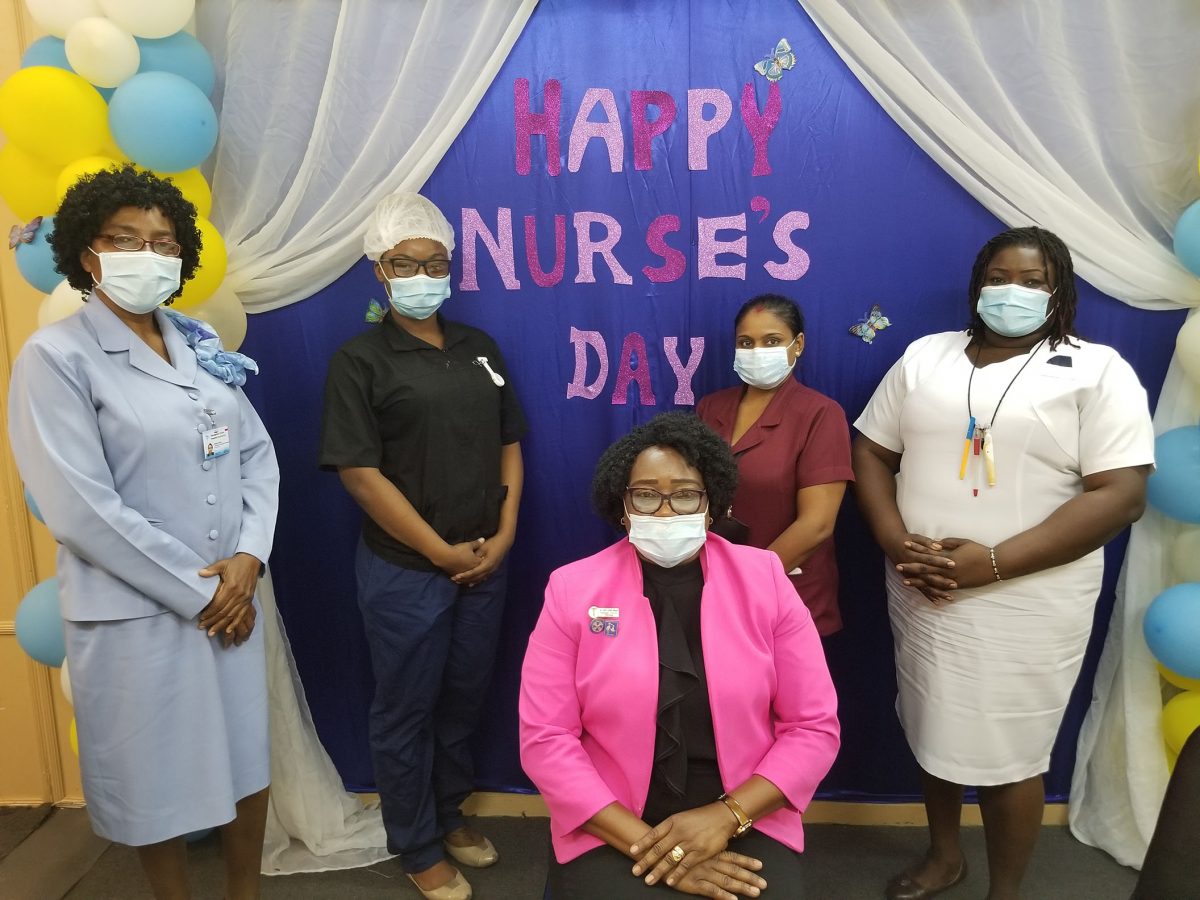
 Guyana and the rest of the world observed International Nurses Day last Tuesday. This day is observed around the world on May 12 each year, to mark the contributions that nurses make to society. This year, there was more appreciation for nurses and the work they do.
Guyana and the rest of the world observed International Nurses Day last Tuesday. This day is observed around the world on May 12 each year, to mark the contributions that nurses make to society. This year, there was more appreciation for nurses and the work they do.
If you have conversations with them you will find there is almost a common motivation—they wanted to give back and care for others. They would tell you how they cry when a patient dies and many times it is their families who help them through it all. But they would also tell you how happy they are when a patient gets well as the stories of their patients live with them.

Assistant Director of Nursing at the Georgetown Public Hospital (GPH) Celeste Johnson-Gordon still remembers the first baby she delivered in Lethem over 30 years ago while GPH’s acting Senior Departmental Supervisor Shivani Ramdihol remembers the 13-year-old who contracted HIV many years ago. She had no children at that time but remembers that she saw her young brothers in him and how she wept for him when she got home that evening.
Brought up in a home with nurses
For Nurse Ramdihol, growing up in a home where both her parents were nurses, joining the profession was natural progression. She describes the profession as “very caring” and one where you can “actually bring happiness to people” and not just the patients, but their families and even entire communities.
Sixteen years after joining the profession she has not regretted following in her parents’ footsteps. She was a very young nurse when she encountered the teenager who tested positive for HIV.
“At that time, I had three brothers and it really… I went home and I cried because I said imagine children at his age. He wasn’t born with it. It was very heart rending…,” she said of the experience during an interview with Stabroek Weekend. But as the years went by, she had to find ways of dealing with her emotions and she said at times she believes nurses become robotic. “You see people pass away and it just becomes a norm. Some of them you go in a corner and cry but then you have to get yourself back together,” she noted. She deals with the paediatric ward and it is particularly hard when children die. Also, a midwife, Nurse Ramdihol has worked in the neonatal intensive care unit and she found that experience difficult.
“It is heart rending to know that a mother delivered and then she can’t get her baby because of certain complications the baby would have died,” she said.
“I always wanted to be a nurse. Since I was a child, I wanted to be a nurse and listening to stories from my parents and my aunts telling me, ‘oh you used to be so nurturing’, and if anyone had a cut I was the one to attend to it. So, for me it has always been a dream to become a nurse and that is why I choose this career,” was how GPH’s staff nurse/midwife Niketa Wickham described her motivation for joining the profession.
As a junior manager with ten years of nursing under her belt Nurse Wickham manages her ward and ensures its operation but she still does deliveries and interacts with patients. She sees midwifery as a “completion of a nurse” as she has always heard that one is not a “complete nurse if you haven’t done midwifery”.
She has had her difficult days as a nurse, but she said with the years she, like many, has learnt not to take her work home.
“You learn that at the end of the day, this day provides for its own set of responsibilities, so you have to know to leave it there. But you don’t start off in nursing knowing that. As you go on then you understand,” the mother of two said.
Even now, though Ramdihol said many times she goes home and cries; as a supervisor, she does not want to show her emotions in front of the junior nurses whom she must support, so, it is her husband who sees her crying.
‘Passion’
For the 34-year veteran Sister Johnson-Gordon it was at around the age of 16 that she fell in love with nursing while visiting her sick grandmother at the Suddie Hospital. More to the point, she fell in love with the nurses.
“I just admired how they would go about their chores in their lily-white uniforms, their caps and their aprons and their lily-white shoes…,” she recalled of the experience.
Her grandmother subsequently died, and her grandfather went to live with them. She took pleasure in taking care of him. A friend was given an application form to enter the profession, but she did not want to leave her lucrative employment at the time and the young teenager grabbed the application form and applied.
The rest is history.
“I started off as a nursing assistant,” she said candidly and later added that it is never a matter of where someone starts.
“It doesn’t matter where you start it is where you want to go because there are different levels of nursing… you could elevate yourself…, “ she said, pointing out that there are now degrees, masters and even doctorates that one could study in nursing.
“The love and the passion,” are what kept her going for 34 years with “no break in service. I didn’t go anywhere I stayed right here.” GPH, except for a few years she spent in Lethem and Suddie, has been like a home for Sister Johnson-Gordon and she boasted that she has worked in all of the wards of the hospital.
She recalled the experience of being a midwife in Lethem as “challenging” as she had to traverse across the savannah attending to patients, sometimes late at night or early in the morning.
“It was anytime they called I had to go. It was in the deep savannahs… and you deliver right there. I tried to walk with my kit with every possible thing…,” she said adding that sometimes she travelled for hours to reach a patient.
There was one experience where the vehicle she was travelling in became submerged in a creek and she along with her junior nurses had to join the driver in pushing the vehicle. That day they left at 4 pm and did not get back to the hospital until 9 am the next day. It also rained and she recalled that they completed most of the journey in wet clothes. But when she got to a mother lying in pain waiting to be delivered, it was all worth it. There were other times when she pushed vehicles out of the mud, but those experiences never daunted her passion for the profession.
“They made me a better midwife. I gained confidence. I gained strength. It was a good two years,” she said of her Lethem Hospital experience. She later returned for a year, when she responsible for the entire region and, according to her, combined they were “three glorious years”.
‘We know what we do as nurses’
All three of these nursing professionals are well aware that they play second fiddle to doctors who are seen as the miracle workers.
Nurse Ramdihol said she has learnt to overcome this, because, “we know what we do for patients.
“Our profession is not about the money that you get but it is the job satisfaction. When you can see a patient walking down the road or a mother who years after… You know, I was down Regent Street and she was like, ‘Nursie, nursie, this was the child you delivered,’ and the child bigger than me [in size],” she said laughing.
Those are the little things that mean a lot to her and other nurses and while the doctors are always “up at the top and we are way below”, as it is way the public sees them, “we are always there 24/7”.
Sister Johnson-Gordon wants the public to recognize nurses more for their invaluable service and she noted that with the advent of the COVID-19 pandemic and them being frontline workers they have seen more appreciation from persons.
“I don’t know but maybe it had to take COVID for us to be recognized as frontline workers,” she added, even as she encouraged persons to stay home and take the necessary precautions to protect themselves.
Suspected COVID unit
For young GPH Registered Nurse Napeth Dey, when she was informed that she was going to have to work at the area where suspected COVID-19 persons would have to await their results she was hesitant.
“At first, I was a bit skeptical because of lack of knowledge but as I began to read and do my own research, I was like, this is not so bad after all. Now I am a bit more relaxed because every day we are getting more information…,” the nurse said.
She spoke of many of the patients she interacts with in that unit being very fearful and some shedding tears as they spoke about their dependent children. To help them, she said, they have to build a trust relationship between patient and nurse. “We do not give false hope, false information but then we let them know it is not the end of the road if you have COVID, you will not automatically die.”
She has been a nurse for almost five years, and she recalled that it was her sister who was studying to become a doctor, who first for her attention when she discussed her studies with her. Then, her passion was to become an economics teacher, but when her application was unsuccessful, she applied to become a nurse. “I got through and from then to now it has been a great experience,” she said.
‘Panic’
Meanwhile Sister Johnson-Gordon said the GPH has been following the WHO/PAHO guidelines for COVID-19. She noted that as the main public hospital “everything comes here” and they are trying to ensure that they flatten the curve.
She recalled that when the first case of COVID-19 was identified, there was panic among nurses especially when they had to open the COVID-19 Intensive Care Unit to which some 13 nurses are attached.
But the panic subsided, and she said eventually they actually got volunteers to work at the unit.
It took nursing consultant Dr Mandy La Fleur, who is attached to the Ministry of Public Health, to help the nurses through that process of accepting their responsibilities and being open to working with COVID-19 patients.
There were a lot of departments that were in a panic and Sister Johnson-Gordon recalled that the dialysis department was one of those. The nurses at the unit were reluctant to treat a suspected COVID-19 patient who needed dialysis. But following Dr La Fleur’s training there were four volunteers that said afternoon to treat the patient.
Dr La Fleur explained that she was asked by Minister of Public Health Volda Lawrence to give support to the hospital in its fight against COVID-19 especially in the area of nursing.
She said a nursing guideline was developed for the management of COVID from which the training was derived. She said the training is geared towards sensitization and bringing information to the nurses also with a behavioural change component.
“Because we understand the fear and the anxiety as a result of lack of information. We try to provide that information in the training and then work the behavioural component into it,” Dr La Fleur said.
She explained that getting the nurses to understand how the disease is transmitted was very important as it can only be transmitted through the respiratory tract and when they understood this it allayed many of the nurses’ fear.
“The staff were scared because they had suspected or confirmed cases coming to them with little or no information and we tried to bridge that gap and provide the communication and allay those fears,” she added.
Referring to the case mentioned by Sister Johnson-Gordon, Dr La Fleur pointed out that the individual had two negative test results and still the staff initially did not want to treat him at the dialysis unit.
“They were very fearful, so… we intercepted that and provided the information… and we asked them what if the patient was your relative what would you have done?” she said adding that the training has seen tremendous positives.
“We are having nurses who are coming forward not to say ‘I want to join nurses who are in direct contact with those patients to take care of them because this could be my relative, this could be my friend’,” she added.
Training has also been developed for maternity nurses and the midwives are on board and they have now developed an isolation area in the event there is a positive pregnant woman.
They have also had web training for regional health workers and the trained nurses are also volunteering to train their colleagues.
Nurses at GPH are ready to take the fight to COVID-19, and hopefully, very soon, nurses around the country will be as well. The unsung heroes are as usual involved in heroic exploits.