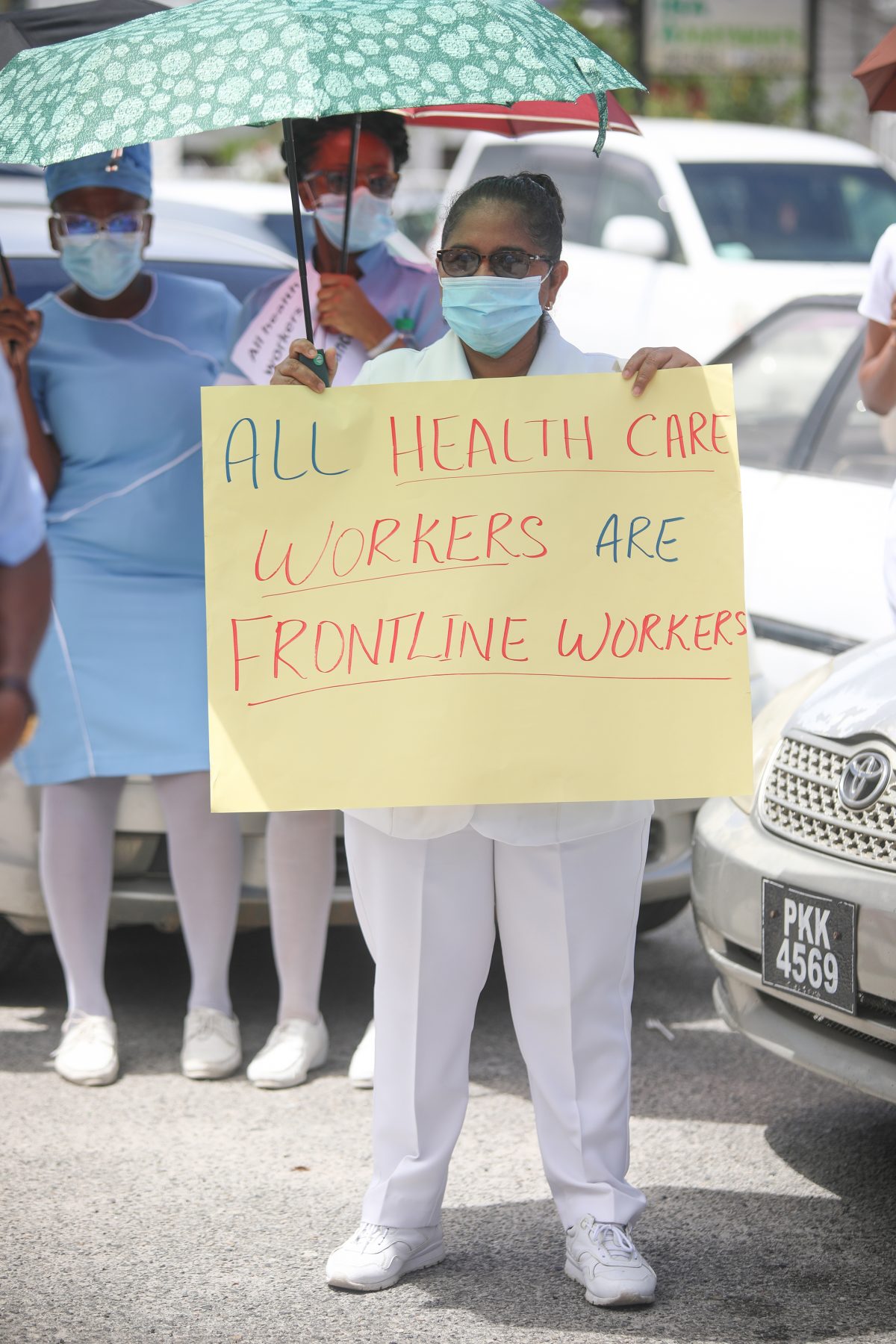
Despite government’s threats of sanctions against health workers who have been protesting for better benefits for those on the frontline in the response to the COVID-19 pandemic, the Guyana Public Service Union (GPSU) yesterday signalled that it intends to proceed with planned industrial action this week unless its demands are met.
“Until they [our attorneys] say otherwise, the 72-hour ultimatum remains in place,” acting General Secretary of the GPSU Kemton Alexander told Sunday Stabroek, while maintaining that the union has followed the necessary legal processes for registering a “grievance.”
The union has asked for a “positive response” towards resolving the issues.
While saying that government could negotiate under duress, Attorney General Anil Nandlall on Friday warned the GPSU that frontline health workers could face sanctions, including criminal charges and the termination of their work contracts, if they continue to engage in what he maintained were illegal ongoing protests.
“Unless these protest actions cease immediately and the procedures outlined by the law are invoked, the government will have no alternative but to consider certain options, including but not limited to, the institution of criminal charges, dismissal, termination of contracts of employment, suspension of the collective labour agreement with the GPSU and the suspension of the deduction of the Union dues for and on behalf of the Union,” Nandlall wrote in a letter to GPSU President Patrick Yarde, in wake of the threatened strike.
‘Fire with fire’
In response, some health workers who have been protesting for better working conditions yesterday accused Nandlall of exacerbating the current unrest rather than mitigating it. There have been protests by staff from the major public hospitals.
“Personally I believe he is trying to fight fire with fire instead of trying to extinguish it. The nurses have already made up their minds to face whatever consequences come their way, so by issuing another threat it basically just gets persons angrier,” one nurse, Jeanel Lewis, told Sunday Stabroek in an invited comment.
She added that a proper response from government to the situation would have been to ask for a meeting and hear the nurses’ concerns about what they wish to have and meet them halfway.
Lewis, a nurse assigned to the Cardiac Intensive Care Unit of the Georgetown Public Hospital (GPH), said she is tired as the issues being raised were problems before the pandemic and have since gotten worse.
Since the start of April, some health workers at the GPH highlighted to management by way of a letter that it had become riskier for them to come to work every day under the prevailing circumstances.
They cited a case where following direct contact with a COVID-19 patient, who subsequently died, 25 staff from the male medical ward were asked to quarantine.
Lewis shared images of a medical gown that is part of her personal protective equipment (PPE) and which she had been asked to take home and sanitize so that it could be reused. She lamented the limited definition of a frontline worker being used by the health sector.
“Only persons working in the COVID-19 Unit are being paid risk allowance. Other workers like myself who are in close contact with patients who are admitted to the unit and then swabbed are placed at risk when the results comes back positive. With no risk allowance, many units have been complaining about not being adequately supplied with PPE. The sisters in charge of the units have to walk to various units seeking assistance for staff to function,” Lewis explained.
She along with other health care workers have used their social media to share their struggles as they fight to be heard.
One such worker, a doctor attached to GPH, shared that during a 12-hour shift in the Emergency Room her supervisor “had to beg for adequate masks”.
“Our overalls are short in stock and our patient load is high. In a 12-hour shift I saw more than 80 percent of my patients as possible COVID-19. I had a patient boarding for over 24hrs because there was no space on the ward. I had a few sicker patients who had to stay at another hospital with less care because we had nowhere to put them. I had a baby not seen for a while because there was no bed to examine him,” she lamented.
“We are tired. My nurses are underpaid, risk allowance is minimal if at all then they are told they cannot protest. If you continue to overwhelm us, underpay us and jeopardize our health…you will lose us!” she concluded.
Lewis shares these sentiments. She indicated that at GPH the risk allowance is $12,000, while gross salaries for nurses range from $74,000 to $104,000. The nurses are asking for an increase in risk allowance to $50,000 and a significant increase in the base salary as well.
“Ministry nurses earn far less. A Ministry of Health registered nurse earns a GPHC Nursing Assistant’s salary. GPHC pays more than Ministry of Public Health because there is no pension plan nor gratuity,” she explained.
A chance
But the government and the GPH’s administration maintain that the health care workers failed to register a “grievance” with the relevant authorities.
Minister of Public Service Sonia Parag has repeatedly stated that she has found no evidence that GPSU gave her Ministry or the Ministry of Labour the one-month period required by law to address the issue.
She announced during an interview with the National Communications Network (NCN) on Friday that the protests were “politically instigated” by the union and claimed that both GPH and Ministry of Health earlier this year made request for increases allowances. “Then Minister of Finance Winston Jordan refused. It was flatly refused and the union did nothing,” she claimed.
It is not clear if the union was ever aware of this refusal.
Chief Labour Officer Charles Ogle, who appeared with Parag, said that there was no official notification received by his office about a grievance in the public health sector.
“You only have these actions [protests or strikes] if there is a stalemate. The law states you have to give management a chance to address your concerns,” he said.
Asked if a letter written on January 24th, 2019 by the union could not be counted as notice, Ogle said no.
He explained that since a meeting was held in February, 2019, and committees were formed to resolve the issues the ultimatum of the January 24th letter could not still be active.
According to Ogle, in the case of GPH, where the union had written to management on April 2nd, 2020 an April 3rd, 2020 meeting similarly negated its effect. “The engagement twice for the same issue means the ultimatum is no longer valid,” Ogle concluded.
Alexander yesterday disagreed with Ogle.
“I don’t agree with him. My understanding of industrial relations will not allow me to agree with him,” Alexander said last evening.
He explained that while a meeting was held in February, 2019 and three committees were formed, they never completed their duties so they could not have negated the ultimatum.
Additionally, according to Alexander the April meeting with GPHC administration “ironed out” a few things not all and even those measures agreed on have not been implemented.
“Those things are inconclusive so our ultimatum still stands,” he said, while adding that the union had also reached out to Public Service Permanent Secretary Soyinka Grogan since the new government entered office.
GPHC has publicly stated that amicable agreements were reached on issues such as providing appropriate training to all staff members to combat the COVID-19 virus; providing transportation to take employees to and from work; paying risk allowances to all staff members who are directly involved in the treatment and care of COVID-19 patients in accordance with Circular Memorandum PS: 20/19 dated December 12, 2019; providing adequate and appropriate Personal Protective Equipment (PPE); providing psychological support to employees who are affected by the COVID-19 virus; providing meals and beverages to employees directly involved in the treatment and care of COVID-19 patients and at COVID-19 screening/triage sites; continued payment of salary to employees who are on extended sick leave due to COVID-19; providing care packages to employees who are affected by COVID-19; and providing free housing to staff members who perform duties in the COVID-19 Isolation Intensive Care Unit.
While Alexander could not remember every issue agreed on, he singled out “risk allowance,” stressing that while the hospital has claimed that persons who had been in contact with patients will be provided risk allowance, this is not the case.
“Everyone working in a medical institution is a frontline worker because everybody is at risk,” he stressed, while explaining that clerical staff at the hospital as well as nurses and doctors outside the COVID-19 unit are being infected.
The term frontline worker has to be redefined, he maintained.
‘Sick out’
He went on to confirm that several nurses attached to the Cardiac Intensive Care Unit of the Georgetown Public Hospital Corporation (GPHC) reported “sick” Friday evening.
He noted that while he did not have the number of nurses who participated in the “sick out,” he knew that the unit is usually staffed around five.
With the union threatening a full blown strike from October 7th, GPHC has moved to put measures in place to mitigate its impact.
A memorandum to department heads from Director of Medical and Professional Services Dr Fawcett Jeffrey suggested that emergency care could be reduced so as to all remaining staff to participate in essential inpatient care.
Other measures suggested include identifying the personnel who will be willing to work and facilitate medical care to persons seeking same, re-arranging staff members who are willing to provide essential services to the inpatients that may have been unfortunately inconvenienced by the strike actions and reducing the inpatient population by discharged.
“All patients who will not be adversely affected will be given a home care plan until the situation normalizes,” he suggested in the memo, while adding that all outpatient activity will be suspended or referred with provisions in place to allow for education, advice, repeat treatment to persons in need.
“In the absence of Nurses in Clinic areas, the Wards or Operating Room, doctors will be asked to assist with basic interventions like medication dispensation, vital signs and dressings on patients who for one reason of the other could not be discharged or referred to another institution for care. Teams should be created with the available personnel to identify who will be responsible for which duties to allow for patient care to continue in crisis mode,” the memo further added.
Family members are also likely to be called on to assist with visitation to be eliminated except for family members attempting to remove their patients from the hospital, and a willing relative who will assist with the care of the patients remaining. This care is to include showering, feeding and other physiological needs.