-Auditor General’s report
A report by the Auditor General’s Office on the maternity unit at the GPHC from January 2019 to June 2020 revealed a persistent shortage of healthcare personnel, particularly nurses and midwives, compounded by a lack of comprehensive staff training and inadequate standard operating procedures.
This report dated September 2024 was tabled in the National Assembly on Thursday.
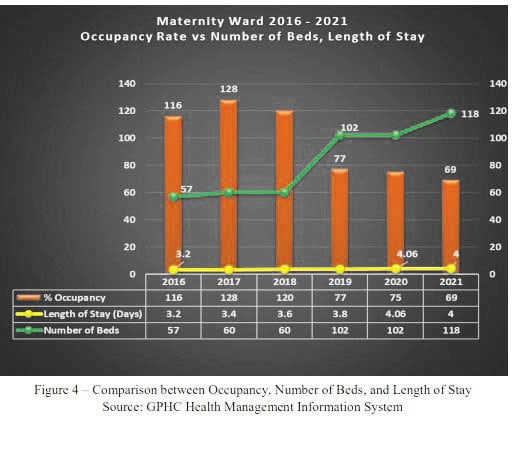
Despite these challenges, the report indicates some progress at the Georgetown Public Hospital (GPHC) regarding bed availability. The average bed occupancy rate in the Maternity Unit was 76% during the audit period, a significant improvement from previous years when overcrowding peaked at an alarming 121%. This reduction has allowed the hospital to better manage patient flow and adapt to fluctuations in demand.
However, the report outlined a range of troubling deficiencies. Throughout the audit period from January 2019 to June 2020, GPHC’s staff levels were approximately 63% of the proposed capacity. This shortage, the report said had serious implications for patient care, potentially leading to poor health outcomes, including increased risks of maternal mortality, which was estimated at 110 to 112 deaths per 100,000 live births in 2019 and 2020.
The Auditor General’s findings further said that the GPHC had not conducted a needs assessment to identify necessary personnel and equipment, potentially leaving patients without essential treatment. The report criticized the management for failing to ensure that established policies and procedures are consistently followed.
The report emphasized that the absence of a comprehensive manual of administrative procedures has left staff without clear guidance in their roles. Ward protocols that do exist were outdated and inadequately communicated, leading to inconsistencies in patient care. Furthermore, the audit revealed that unserviceable equipment cluttered key areas of the Maternity Unit, posing additional safety risks.
The audit also revealed that staff training needs were not sufficiently evaluated, resulting in gaps in the knowledge and skills essential for effective patient care. GPHC management recognized this issue and expressed their commitment to implementing training programmes to address these deficiencies.
While the Maternity Unit was responsible for over 40% of the country’s annual births—approximately 6,000 per year—the report stressed that the quality of care provided had not kept pace with demand. Stakeholders, including parliamentarians and the public, had voiced significant concerns regarding the Unit’s operational capacity and the effectiveness of its patient management systems.
Concurrently, the GPHC maintains proper documentation of patient medical histories, ensuring a structured approach to patient care across the admission, treatment, and discharge phases. However, the absence of a formal performance monitoring system means that the hospital is ill-equipped to identify and address ongoing deficiencies.
Lastly, the Auditor General identified a critical deficiency in the Quality Improvement Unit, which lacked a robust system to monitor and evaluate the performance of the Maternity Unit. These findings underscored the urgent need for improvements to ensure a higher standard of healthcare delivery.
The report concluded that GPHC management had not effectively supervised the Maternity Unit, potentially jeopardizing the delivery of quality healthcare. Key recommendations included establishing comprehensive administrative procedures, increasing staffing levels, and creating a robust system for ongoing training of healthcare personnel.
The GPHC management has pledged to implement a series of recommendations aimed at enhancing the oversight and functionality of its Maternity Unit. Management has acknowledged the need for improved documentation of monitoring activities to support informed decision-making among stakeholders.
Routinely presented
According to GPHC’s management, monitoring findings, investigative outcomes, and reports are routinely presented to the Board of Directors on a monthly basis. Complaints and grievances are meticulously tracked and escalated to the appropriate managers, ensuring that these insights lead to necessary departmental improvements.
Management has committed to establishing a more structured process for periodic reviews of operational effectiveness. Although some review mechanisms currently exist, including daily management huddles and other committees, there is a recognized need for a comprehensive approach. Notably, the audit revealed a lack of standardized monitoring tools within the Quality Improvement Unit, particularly concerning the Maternity Unit’s performance metrics.
The Audit Office has also recommended that GPHC management set up a systematic process to evaluate results from monitoring efforts, thereby facilitating timely interventions when deficiencies are identified. Management has responded by affirming that the Maternity Unit is evaluated quarterly under the Service Level Agreement (SLA) with the Ministry of Health, employing various performance indicators related to patient flow, outcomes, and safety. Management noted that while the SLA provides an independent performance assessment, there is an urgent need for comprehensive policies and updated protocols to guide the Maternity Unit’s operations.
The absence of a fully approved manual of administrative procedures was flagged as a significant oversight that could jeopardize the quality of care. Management is now focused on developing a comprehensive procedural manual to meet the requirements set forth by the Health Facility Licensing Regulations 2008.
In response to concerns regarding resource management, the GPHC has stated that an annual budgeting process is in place to evaluate departmental needs. However, the audit emphasized the need for regular assessments of the Maternity Unit’s resources to ensure quality healthcare delivery.
Despite these challenges, GPHC reported that its bed capacity aligns with the average occupancy rate, indicating that the facility can adequately accommodate its patient load. The audit office has recommended ongoing inspections of the hospital’s facilities and equipment to promptly identify and rectify any potential hazards.
GPHC management has expressed its dedication to addressing the audit findings and improving the overall quality of maternal healthcare services, affirming that comprehensive changes will be implemented in collaboration with international partners and internal stakeholders.
On the shortage of personnel, the hospital said: “The GPHC continues to engage the Government of Guyana through the Ministry of Health to mobilize and train additional nurses as the institution grapples with significant shortages due to the global demand for qualified nurses post COVID-19. The institution has also made numerous proposals over the past months for monetary and nonmonetary incentives for nurses. To date, the institution has received some nurses from the MoH, the regions and Cuba, and is currently awaiting some additional registered nurses. Independently, the Corporation has embarked on numerous initiatives for the recognition of its nurses including rewards and recognition programmes such as the Daisy Awards, celebration of International Nurses’ Week and the provision of specialised training programmes. GPHC’s management continues to explore additional incentive programmes and opportunities to attract and retain nursing personnel”.